
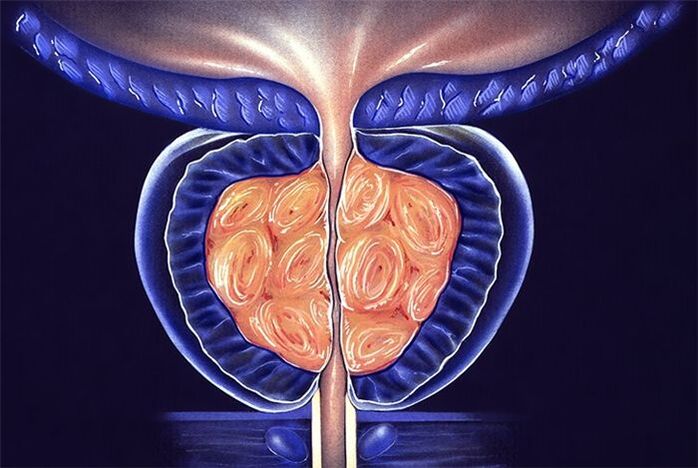
Inflammation of the prostate today is a leader in the group of male diseases that are predominantly sexually transmitted. Its complications threaten infertility, decreased libido, and impotence.
Symptoms of prostatitis are not just pain, urination disorders, and inflammation of the spermatic cord. The most dangerous consequence of advanced inflammation can be cancerous degeneration of the prostate gland. Whereas a timely diagnosed pathological process is easily stopped.
Signs of the disease
If a man discovers at least two of the following symptoms of prostatitis, he should immediately contact a qualified specialist:
- Disorder of urination with the occurrence of an intermittent, weak stream of urine, unusually short, causing splashing, difficulty and pain before urination. Frequent urge to empty the bladder occurs mainly at night.
- Soreness, which is localized in the lower abdomen, radiates to the scrotum, perineum, and rectum.
- Sexual dysfunction.
- Problems with ejaculation, changes in sperm (consistency, quantity).
Acute prostatitis
The disease begins with a sharp rise in temperature (up to 40 degrees), painful headache, and fever. The symptoms that appear are accompanied by pain in the groin, perineum, back, discharge from the urethra, frequent urination and a constant urge to urinate.
Emptying the bladder occurs with a delay and a burning sensation. The urine itself becomes cloudy and may contain blood. Irritability and fatigue occur.
The outcome of acute prostatitis can be complete resolution of the process (if treatment is started in a timely manner). Since changes occur in many pelvic organs, they cannot be left to chance, otherwise the corresponding complications will arise:
- Vesiculitis is an inflammation of the seminal vesicles, the cause of the appearance of pus in the sperm, which not only reduces the quality of the ejaculate, but leads to loss of reproductive function.
- Colliculitis - inflammatory changes in the seminal tubercle become the reason for the development of severe pain during sex, interruption of orgasm, and impotence of a psychological nature.
- The formation of an abscess in the body of the prostate, its rupture, and purulent damage to the rectum leads to an exacerbation of symptoms, severe intoxication of the body, even death.
- Stagnation in the tissues of the prostate leads to changes in their structure, disruption of innervation, blood supply, both to the gland itself and to organs located nearby, with disruption of their functions. The erection becomes insufficient for full sexual intercourse, premature ejaculation and prolonged sexual intercourse without orgasm are observed.
- Cicatricial changes in the gland and spermatic cord lead to infertility, a decrease in the quality of sperm, and sperm motility. Narrowing of the urethra interferes with the normal process of urination; obstruction of the bladder can cause acute urinary retention, requiring emergency surgical care.
Chronic prostatitis
The main feature of the disease is the vagueness of clinical symptoms with a long, persistent course of the process. More often, the chronic form occurs independently, as a primary pathology against the background of stagnation of blood in the vessels (prostatosis), abacterial prostatitis.
The main symptoms of chronic prostatitis are:
- fever;
- pain occurs in the scrotum, perineum, anus, back;
- urinary disturbance;
- mucous or mucopurulent discharge from the rectum, urethra, even in the absence of urination or defecation;
- erectile dysfunction, painful ejaculation, interrupted sexual intercourse, prolonged intercourse without a feeling of satisfaction.
Inaction and improper treatment of chronic prostatitis can cause complications:
- Infertility is the result of chronic inflammation in the spermatic cord, vesicles, testicles, and their appendages.
- Cystitis, pyelonephritis (other diseases of the genitourinary system) are a consequence of hematogenous and mechanical spread of microbes.
- Sepsis.
- Persistent decrease in immunity.
- Untreated prostatitis can cause cancer in 35–40% of cases.
Diagnostics
The clinical picture of the disease is typical, so the diagnosis is not difficult. It is performed by a urologist based on medical history, examination of the patient, laboratory minimum using the most modern medical devices:
- Rectal examination of the gland, taking secretions for examination (culture with determination of sensitivity to antibiotics).
- UAC, UAM, bacterial culture of urine.
- Smear test for STDs, UGI examination.
- Daily monitoring of urination rhythm, measurement of urination rate (uroflowmetry).
- For differential diagnosis, ultrasound or TRUS is performed.
- If it is necessary to exclude oncology, a biopsy is taken, urography is performed, and PSA is determined - prostate specific antigen.
- To diagnose infertility, a spermogram is prescribed - an analysis of ejaculate to determine the fertility of a man.
Based on the results of the patient’s examination, an individual scheme for complex treatment of prostatitis is drawn up. When prescribing drugs, the form of the pathology and the presence of concomitant diseases are taken into account. The decision about where to conduct therapy (inpatient or outpatient) is made by the doctor. The course of treatment is carried out with careful laboratory monitoring of results.

Treatment of acute prostatitis
Acute prostatitis requires bed rest, a special, salt-free diet, and sexual rest.
Methods of course treatment:
- The most effective treatment for prostatitis is etiotropic therapy. If the basis of prostatitis is an infection, a course of antimicrobial agents is a priority, which relieves the manifestations of inflammation.
- Pain syndrome is relieved with analgesics, antispasmodics, rectal suppositories, microenemas with warm solutions of painkillers. NSAIDs may be used.
- Immunostimulants, immunomodulators, enzymes, vitamin complexes, and a combination of microelements have proven their effectiveness.
- Physiotherapeutic methods are possible only in the subacute stage of the disease. They improve microcirculation and increase immunity: UHF, microwave, electrophoresis, laser, magnetic therapy.
- Massage is another effective method of influencing the prostate. It opens the ducts, normalizes blood circulation in the scrotum and pelvis.
- Acute renal filtrate retention can be corrected by catheterization and trocar cystostomy.
- The purulent process involves surgical intervention.
- Psychologist consultations.
Treatment of chronic prostatitis
With a long-term, course (at least a month) effect on the prostate, there is no 100% guarantee of cure. Priority goes to herbal medicines, immunocorrection, changing household habits:
- Herbal preparations are widely used in urological practice. They are able to accumulate at the site of the most active pathological process, protect cells from oxidation, remove free radicals, and prevent the proliferation of glandular tissue.
- Antibacterial therapy is selected individually, based on the sensitivity of microbes to drugs.
- Drugs that enhance immunity not only help to cope with prostatitis, they also correct the negative effects of antibiotics that disrupt the function of the immune system.
- The pain syndrome is relieved by the administration of alpha-blockers and muscle relaxants.
- Prostate massage allows you to mechanically remove the "extra" secretion of the gland through the urethra, improve blood circulation, and minimize congestion.
- Physiotherapy: laser, magnet, ultrasound, iontophoresis, warm sitz baths or microenemas with herbs.
- In severe cases, intravenous fluids with diuretics are indicated. This stimulates abundant urine production, prevents symptoms of intoxication, the development of ascending cystitis, and pyelonephritis.
- For constipation, herbal laxatives are used.
- The urologist and psychologist, together with the patient, develop an individual long-term program of daily routine, necessary rest, diet, dosed physical activity, and sexual activity.
- If the chronic process is resistant to therapy and the outflow of urine is blocked, surgical intervention is prescribed: removal of all affected tissue (transurethral resection of the prostate) or complete removal of the gland with surrounding tissues (prostatectomy). Practiced in exceptional cases, it is fraught with impotence and urinary incontinence. Young people do not undergo surgery because it can cause infertility.
Symptoms and treatment of chronic prostatitis
Many men suffer from chronic prostatitis, but they attribute the symptoms to other diseases or waste time on ineffective treatment. From our article you will learn comprehensive information about this male problem: causes, exact symptoms and diagnostic methods, various treatment methods.
Despite all the successes of modern medicine, diagnosing a disease such as chronic prostatitis causes certain difficulties. This also negatively affects the effectiveness of his treatment.
Causes of chronic prostatitis
The causes of chronic prostatitis are very different. Of the variety of negative factors affecting a man’s health, it is difficult to single out exactly those that provoked the development of the disease. Often this is a complex of situations and circumstances accompanying a man’s life.
The main causes of chronic abacterial prostatitis are the following:
- dysrhythmia (irregularity) of sexual intercourse;
- physical inactivity, which is typical for overweight people;
- long-term stressful conditions;
- the predominance of foods rich in fat in the diet;
- negative impact on the body in hazardous industries.
Chronic prostatitis of the bacterial type is the result of incompletely cured bacterial prostatitis. Or the man ignored the ailments and did not seek help from a urologist. Therefore, no treatment was carried out.
Chronic prostatitis of the abacterial type develops due to exposure to infectious agents against the background of decreased immunity. As a rule, such patients are diagnosed with diseases of the endocrine system.
Factors that provoke the development of chronic bacterial prostatitis are:
- surgical operations on the prostate (if antibacterial therapy was not performed before the operation);
- refusal to use contraception;
- lack of habit of keeping your body clean.
Symptoms of chronic prostatitis
Today there are many myths regarding chronic prostatitis. For this reason, any temporary disturbances in sexual function are attributed to this disease. You can often hear the opinion that decreased libido and erectile dysfunction are due to prostatitis, and if an older man, then to chronic prostatitis.
This is not true, since sexual dysfunction has many other causes, and the main symptom of chronic prostatitis is pain. All other signs can be considered concomitant and indirect.
Chronic prostatitis is often confused with pelvic pain syndrome, since the symptoms of these diseases are largely similar. This is due to the formation of myosfacial trigger zones near the prostate, which appear as a result of injuries and surgical interventions. Pain in these areas can be mistaken for a symptom of prostate inflammation.
In the diagnosis of the disease, complaints of pain and discomfort in the perineum and pelvis, lasting at least 3 months, come to the fore. The pain is localized near the prostate, radiating to the sacrum, rectum, and scrotum. With prolonged exposure to negative factors (carrying heavy objects, excessive physical activity, being on your feet for a long time), the pain intensifies.
A characteristic sign of the disease is premature ejaculation. Patients experience decreased sexual desire and erectile dysfunction. These symptoms are also characteristic of other genitourinary diseases. Therefore, it cannot be said that they are hallmarks of chronic prostate disease.
An important symptom is the fading of orgasm. If the patient begins to notice that the severity of sensations during ejaculation has disappeared, this is a reason for a more attentive attitude to his health and a signal about the need to visit a urologist.
The structure of the inflamed prostate becomes denser, the pressure on the urinary tube increases, and the quality of urination deteriorates. Patients with chronic prostatitis note a frequent urge to urinate at night. The process of urine excretion is accompanied by a burning sensation, stinging, and pain. Urinary incontinence often occurs.
Signs of chronic prostatitis can be expressed in full or partially. Much depends on the patient’s health status and the presence or absence of other diseases. Chronic prostatitis is characterized by a wave-like course, with waxing and waning symptoms. With this disease, the inflammatory process is not acute.
Laboratory research methods
If chronic prostatitis is suspected, first of all they find out what its nature is: bacterial or abacterial. In the first case, it is necessary to identify the pathogen or pathogens and find out which drugs they are sensitive to. To do this, laboratory tests of urine and prostate secretions are performed.
If, after a 10-day period after the DRE, the PSA test shows that the level of prostate-specific antigen exceeds 4. 0 ng/ml, this is a reason to refer the patient for a biopsy in order to exclude an oncological process.
The following research methods are recommended:
- scraping from the urethra;
- general and biochemical urine analysis;
- LHC culture of prostate secretion.
Treatment of chronic prostatitis
Treatment of chronic prostatitis requires an integrated approach. Taking medication alone is not enough. Physiotherapeutic procedures and therapeutic exercises are necessary. In general, chronic prostatitis is difficult to treat and requires a radical revision of lifestyle, changes in habits, and in some cases, a change of job. Urologists insist that only a set of measures will help get rid of this disease completely or ensure long-term remission.
Regardless of whether the disease is bacterial or abacterial in nature, congestion in the prostate played a major role in its formation. The viscous secretion deposited in the ducts of the gland is a favorable environment for the development of pathogenic and opportunistic microorganisms. Therefore, the main attention should be directed to eliminating stagnation.
The issue can be solved by changing lifestyle and including physical therapy classes in the daily schedule.
Complexes of exercises have been developed that are suitable for different life situations:
- for those men who are forced to sit most of the time (drivers, office workers, managers);
- for people with excess body weight;
- for those who do not have time to do exercises.
Having thought about how to treat chronic prostatitis, you need to decide to seriously reconsider your attitude towards your health.
Treatment with medications
For chronic prostatitis, outpatient treatment is mainly carried out. If the pathological process persists and it is not possible to achieve remission using this method, hospitalization is recommended. In a hospital, under the supervision of medical staff, there are much more opportunities for compliance with the regime and monitoring changes in the patient’s condition.
Chronic prostatitis in men develops against the background of endocrine disorders. In this regard, drugs 5-alpha reductase inhibitors and alpha 1-blockers are recommended. They help normalize hormonal levels and eliminate the symptoms of pathology.
An integrated approach includes taking medications such as:
Treatment methods for bacterial chronic prostatitis
Bacterial chronic prostatitis is treated with antibiotics. The most effective drug for a particular patient is determined using a preliminary laboratory study of prostate secretions.
There is no universal medicine to suppress and destroy pathogenic microflora. What helps one patient may not help another. For this reason, there are many negative reviews about advertised medications for the treatment of chronic prostatitis.
The drugs recommended for antibacterial therapy are fluoroquinolones. Most bacteria are sensitive to them.
Treatment with herbal remedies
Many people doubt whether chronic prostatitis can be cured with the help of herbal remedies. The answer to this question was obtained through many years of use of these healing agents in urological practice.
Today the following treatment complexes are recommended:
All these drugs have a beneficial effect on the functioning of the male genitourinary system. Effective treatment of chronic prostatitis is possible provided that urinary function is normalized. The components included in herbal medicines perform this task. They help reduce the frequency of urges and eliminate sluggish stream syndrome.
For patients with chronic prostatitis, herbal mixtures containing pumpkin extract or pumpkin seeds are recommended. The latter have a unique chemical composition and act in three directions at once:
- normalize metabolism;
- strengthen the walls of blood vessels;
- activate blood circulation in the pelvic organs.
Taking herbal medicines cannot be regarded as the main method of treatment. These health-improving agents are considered to be concomitant with drug therapy.
Non-drug treatment
Non-drug therapy methods allow you to act directly on the prostate, increase the concentration of medications in its tissues, and help eliminate congestion.
Today, non-drug treatment focuses on laser therapy. The possibilities of this technique are wide. Under the influence of a laser, the following processes occur in the prostate gland:
- activation of redox reactions;
- blood microcirculation improves;
- new capillaries are formed;
- pathogenic microflora is suppressed;
- The process of cell division is activated, which promotes tissue regeneration.
During the period of research into the effects of laser therapy on patients with prostatitis, a side effect, but positive for treatment purposes, was noticed. Those who completed the course increased potency, eliminated erectile dysfunction, and restored vitality. To achieve this result, it is necessary to use a beam with a specific wavelength. In general, low-intensity laser radiation is used to treat chronic prostatitis.
This technique can have several positive effects:
Patients can, on their own initiative, undergo a course of laser therapy if it is not prescribed by the attending physician.
Surgical treatment of chronic prostatitis
Chronic prostatitis does not pose a threat to the patient’s life, but can significantly reduce its quality. The most serious complication of this disease is the formation of stones in the tissues of the gland. In order to free it from prostatoliths, transurethral resection is used.
The surgical intervention is carried out under TRUS control.
If complications such as prostate sclerosis occur, transurethal electrosurgery is performed. If sclerosis of the bladder neck is observed in combination with this pathology, partial resection of the prostate is performed.
When the seminal and excretory ducts are blocked, endoscopic operations are indicated to eliminate the obstruction of secretion patency. For this purpose, an incision is made into the seminal vesicles and excretory ducts. In case of an abscess, complete removal of the gland is possible.
Exercises for the treatment of chronic prostatitis
There are a number of exercises that are effective in stimulating the prostate, which helps relieve congestion. This complex was developed for patients with hip joint problems. Practice has shown that these exercises are also useful for those diagnosed with prostatitis. Classes can be conducted at a convenient time; the complex will take no more than 15 minutes to complete.
Exercise No. 1
- Lying on a gymnastic mat, stretch both arms up.
- Bend your knees and pull them towards you, simultaneously spreading them in different directions.
- Raise the pelvis as much as they can. Repeat 10-12 times.
Exercise No. 2
Standing on the mat, do deep squats.
Repeat 10-12 times.
Exercise No. 3
- Lie on your stomach.
- Raise one leg up, then the other. Repeat 10-12 times.
Exercise #4
They lie on their side.
When performing this set of exercises, all movements should be smooth. This is the main condition for obtaining a high therapeutic effect.
Treatment prognosis
Few men can completely cure chronic prostatitis. Inflammation of the prostate often goes into a stage of long-term remission. But when conditions arise for the activation of the pathology, a relapse occurs. An exacerbation begins with the occurrence of pain in the prostate. Often they are accompanied by urinary disorders. At the first symptoms of relapse, you should seek help from a specialist.
Patients are recommended to regularly visit a urologist, at least once every six months. With the same frequency, they conduct examinations of the prostate condition and take a PSA test. By systematically monitoring the condition of the gland, processes that provoke a relapse of the disease can be identified in a timely manner. But even with long-term remission there is no guarantee that it will not be disrupted.
The patient must follow recommendations to prevent exacerbations of the disease. It is recommended to balance your diet by excluding fatty and spicy foods. The use of herbal remedies and traditional medicine must be agreed with the attending physician. With this approach, you can minimize the risk of exacerbation of chronic prostatitis.
Is it possible to cure prostatitis yourself?
If there are severe symptoms, it is better to be treated by a specialist; the time factor plays a big role in treatment, since the longer the inflammation lasts, the greater the likelihood of irreversible changes in the organ.
But it’s better to do prevention yourself; no doctor will do it for you.
Avoid hypothermia, stagnation during prolonged sitting, sexually transmitted infections, irregular sex life - all this is the way to effective prevention of prostatitis.























